
Texas Tribune / Azul Sordo
August Johansen appears by the glass door of the birthday venue whereas cradling a balloon on Dec. 9, 2023. He had inoperable mind most cancers and relied on Medicaid to pay for full-time house nursing care from a non-public company to assist his mom maintain him all through years of well being crises. Final December, he turned one among 810,000 youngsters dropped from Texas’ Medicaid program within the earlier 5 months, however was reinstated by his mom’s efforts.
Join The Temporary, The Texas Tribune’s each day publication that retains readers on top of things on essentially the most important Texas information.
An unattainable process. That’s what Randy Fritz was confronted with in the summertime of 1999.
As government assistant to then-Texas Well being Commissioner William “Reyn” Archer III, Fritz had 10 months to create from scratch a brand new statewide medical insurance program for poor youngsters who didn’t qualify for Medicaid.
Why the frenzy? There was public stress to get this system rolling after a recalcitrant Texas Legislature had been gradual to undertake what management Republicans considered an entitlement.
However underlining the urgency was the truth that Gov. George W. Bush had not too long ago introduced his candidacy for president — and his allies on either side of the aisle within the Legislature knew {that a} profitable program would give him a lift if he made it by the primaries to turn out to be the Republican nominee, Fritz mentioned.
On the time, the large Texas Kids’s Well being Insurance coverage Program, or CHIP, existed solely on paper, the Legislature having simply handed it weeks earlier because the state model of a 1997 federal program.
These sorts of applications can take years to create and construct up, however Fritz and his counterpart on the company, Texas Well being and Human Companies Fee, needed to get it off the bottom by spring 2000 and ship gangbuster enrollment numbers in a couple of months, Fritz recalled.
In California, which on the time had a inhabitants of 33 million, it took two years to enroll 400,000 youngsters. Fritz’s directive from state price range leaders, who had been additionally Bush allies, was to ultimately enroll practically half one million youngsters within the first 18 months.
Fritz figured the tight deadline was being employed as an efficient method to guarantee that “we went bananas with the enrollment” in time to get adequate numbers to make use of within the marketing campaign, he recalled in an interview Monday with The Texas Tribune.
“We had been advised in no unsure phrases (by a robust Democratic lawmaker who labored on Bush’s marketing campaign group) that our careers would endure if we didn’t ship,” Fritz mentioned. “He supplied no context or clarification for that directive, however we didn’t want that. We knew why he was placing the screws to us.”
Regardless of the motivation, what adopted was a robust illustration of what a state can accomplish when the purpose is to cowl as many Texans as attainable in as brief a time as attainable.

Texas Tribune / Azul Sordo
Erica Olenski Johansen helps August brush his hair earlier than his party.
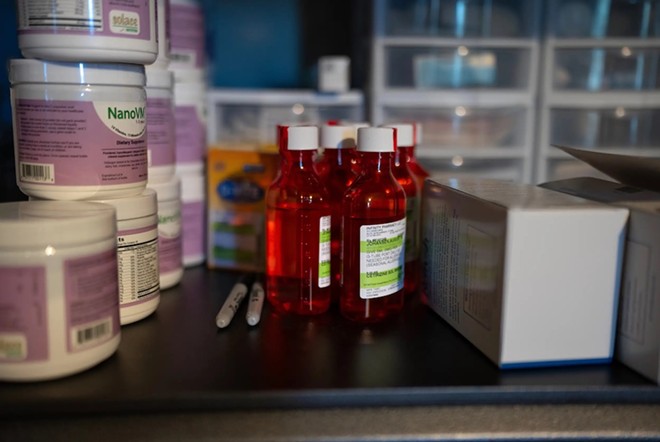
Texas Tribune / Azul Sordo
Medicines and different medical provides line a shelf within the “sport room” of August’s house.
1 / 4 century later, the state has confronted a special large problem. After going years in the course of the pandemic with out ending Medicaid and CHIP protection for anybody, Texas Well being and Human Companies started the method final spring of rechecking the eligibility of anybody on the rolls. Some 2.1 million folks had been dropped at the very least quickly as of late February. Solely 700,000 had been decided ineligible — the opposite greater than 1.3 million who misplaced protection as a result of the state couldn’t affirm their eligibility.
State officers mentioned they labored exhausting to maintain eligible folks enrolled, and employed new employees to get the job accomplished. However advocates for the poor and disabled say different states did extra — they usually discovered themselves wishing for a 1999-like effort from Texas once more.
“It was a situation the place Democrats and Republicans and the governor, particularly, mentioned, ‘That is what must occur for kids. We will get some bureaucrats to determine the best way to really operationalize it. And we’re not going to fret about all the main points. We simply know that the job is getting as many youngsters enrolled for that program as attainable as a result of they want it. It is essential,’ ” Fritz mentioned.
What was at stake in 2000
From the advocates’ viewpoint, success in 1999 additionally meant that Texas — which was and nonetheless is the state with the best fee of uninsured youngsters — would lastly be addressing an pressing want.
Good enrollment numbers would additionally give Bush a wanted “compassionate conservative” counter to then-Vice President Al Gore, the Democrats’ frontrunner for 2000, who had turned the wildly common 1997 bipartisan federal youngsters’s medical insurance laws right into a compelling marketing campaign message.
Fritz mentioned it was clear that if the state’s well being and human companies staff screwed up the rollout, “we might be crucified” each by these with political plans driving on it, and maybe by a public relying on them to get it proper.
Pete Laney, a Panhandle Democrat who was state Home speaker on the time — throughout which each statewide workplace holder was a Republican — mentioned that whereas this system had its detractors, it usually had bipartisan assist.
“It was a public relations star for some people, it was good authorities for some people, and it was, ‘It satisfies my constituents’ for some people,” Laney recalled.
Then-Well being and Human Companies Commissioner Don Gilbert and Archer, gave the state’s well being commissioner, Fritz and others carte blanche to determine issues like the best way to construction this system, which suppliers to incorporate and which contractors to rent for jobs like software program design.
Public consciousness campaigns had been mobilized. Straightforward-to-follow, illustrated utility types had been designed, and processes that helped candidates bypass lengthy arduous in-person interviews had been put in place. State staff and volunteers fanned out throughout the state to teach Texans about qualifying for protection.
It labored.
The state’s enrollment marketing campaign started in Might 2000. By the point Bush confronted off towards Gore within the Oct. 11, 2000 debate, that they had enrolled 87,000 youngsters within the first 5 months — a reality Bush was in a position to boast about. (Bush mentioned 110,000 however was later corrected in follow-up statements.)
By the point September 2001 got here round a yr later, the brand new Texas program had reached full enrollment with 428,000 youngsters.
That’s a mean of practically 800 youngsters per day, a triumph for the politicians who wanted a win — and a heady victory for the social advocates who had lengthy been pissed off by the the state management’s lack of power behind addressing the uninsured disaster.
Had this system saved tempo with the California timeline, which was typical of the rollouts in different states, it could have taken the state till 2004 to achieve that stage of enrollment.
“It was a beautiful time,” remembers Anne Dunkelberg, a retired well being coverage skilled with Each Texan, a progressive assume tank in Austin, who was concerned within the preliminary enrollment push. “We had each an enormous pent-up demand for CHIP, and we had actually sturdy, good-faith permission to attempt to drive up enrollment. It was clear that they had a giant, shiny inexperienced mild to do it, and do it aggressively, and do the very best job they might. The outreach to get CHIP enrollment going was an instance of how Texas can clearly do a bang-up job in the event that they selected to.”
‘The surroundings is flipped’Some 20 years later, HHS – the identical state company that was tasked with masking as many youngsters as attainable in the course of the genesis of CHIP – faces scathing criticism for the best way the company has dropped tens of millions of Texans from the Medicaid and CHIP rolls
The method has led officers on the company to rent extra staff and promise higher effectivity sooner or later because the “monumental process” winds to an in depth.
The state has a Might 31 deadline for the year-long technique of updating its rolls within the aftermath of the COVID-19 pandemic, throughout which period federal rules barred states from eradicating folks from Medicaid or CHIPs. Some 6.1 million Texans had been in a position to entry well being care repeatedly, a 50% improve from the everyday estimated 4 million recipients.
However when these protections had been lifted a yr in the past, the state started rechecking the eligibility of all adults and kids on Medicaid and CHIP and requiring everybody to reapply for advantages by a system that had not dropped anybody for the previous three years.

Texas Tribune / Azul Sordo
From proper: August and his older brother Bryant play a sport on his toy digicam.

Texas Tribune / Azul Sordo
August opens his birthday presents whereas surrounded by mates, a couple of with comparable diagnoses, on Dec. 9, 2023. It was his first party — August spent three of his 5 birthdays within the hospital.
Officers at Texas Well being and Human Companies, which oversees Medicaid/CHIP applications, say they are going to seemingly full the duty a couple of weeks early. The rolls have returned to pre-pandemic ranges, with simply over 4 million folks nonetheless on the applications.
Within the months because the state launched this “unwinding,” critics have mentioned it’s being accomplished too rapidly and has resulted in too many certified folks being dropped and dropping important protection.
It has been “a monumental process” that exposed areas the place the state may enhance for future comparable endeavors, mentioned Tiffany Younger, an HHS spokesperson.
“We now have discovered many classes from these efforts, not simply operationally, but in addition the best way to higher talk with suppliers and purchasers,” she mentioned. “Our nationally acknowledged outreach marketing campaign and ambassador community of neighborhood suppliers and stakeholders has constructed a powerful basis for us to maneuver ahead.”
Lawmakers final yr earmarked funding for HHS to rent extra eligibility staff to assist with the workload created after they started the unwinding. HHS has been in a position to fill some 97% of these positions, and has additionally leveraged exterior contractors, expertise and elevated coaching to fulfill the workload, Younger mentioned.
To this point, Texas has a internet Medicaid/CHIP enrollment decline of 31.6% — second highest decline within the nation. That quantity displays individuals who had been disenrolled in the course of the unwinding course of, new folks coming into this system and those that re-enrolled inside a short while after being dropped, a dynamic generally known as “churn.”
When the state couldn’t decide whether or not an individual was eligible, the individual was dropped from the rolls. That may occur when folks don’t obtain or reply to renewal notices or will not be clear on what’s required to resume. It may possibly additionally occur when enrollment staff can’t course of the applying in time.
“The principle concern with procedural disenrollments is that many individuals dropping Medicaid for these paperwork causes should still be eligible and don’t have one other supply of well being protection,” KFF researchers wrote in a latest report.
Younger mentioned that her company is continuous to hunt methods to make the method simpler and extra environment friendly.
“We’re actively engaged on extra alternatives to additional streamline and automate our eligibility processes,” she mentioned.
For these involved in regards to the uncovered-but-eligible Texans with out Medicaid, that may’t come too quickly.
In response to a latest report by Texas 2036, an Austin nonprofit assume tank, practically half of all uninsured youngsters in Texas are certified for CHIP or Medicaid however will not be enrolled.
Texas has notoriously tight restrictions on who could use Medicaid. The overwhelming majority of recipients are low-income youngsters or medically advanced youngsters. It additionally covers new moms below a sure revenue stage and a few low-income adults with disabilities. Most Medicaid recipients are indigent youngsters of colour.
The restrictions have served to maintain the rolls low, however the lack of eligibility necessities is just a part of the explanation Texas has decrease participation.
“It is very attention-grabbing to really lower Medicaid eligibility or lower Medicaid advantages,” Dunkelberg mentioned. “However you possibly can have an enormous impact on lowering Medicaid enrollment by limiting outreach, limiting utility help, making it tougher to get enrolled and to remain enrolled, whether or not by state regulation or under-the-radar company actions.”
Beneath Republican Govs. Rick Perry and Greg Abbott, administrative processes have been “dramatically weaponized” as illustrated by not simply the present unwinding however by declining numbers and growing crimson tape hooked up to the applications each by company actions and legislative inaction, Dunkelberg mentioned. Abbott’s workplace didn’t return a request for remark.
As examples, she pointed to how modifications in company guidelines, like an absence of deal with the best way to higher educate immigrant dad and mom about the fitting to Medicaid and CHIP for US residents and immigrant youngsters who’ve authorized documentation can have nice influence, advocates say.
Shedding a important perform
For a daunting second final summer season, 5-year-old August Johansen was one of many youngsters to lose protection.
The McKinney boy had inoperable mind most cancers and relied on Medicaid to pay for full-time house nursing care from a non-public company.

Texas Tribune / Azul Sordo
August friends by the window of the birthday venue as members of the family arrive. There are solely a handful of youngsters at his celebration— most are lecturers, nurses and household mates who’ve been with Erica and August by his remedy. In December, he turned one among 810,000 youngsters dropped from Texas’ Medicaid program however he was ultimately re-enrolled.
He had been getting care by a particular Medicaid program for “medically dependent” youngsters, which lined youngsters like him even when their household’s revenue didn’t qualify them for Medicaid or CHIP.
August had a lot of well being challenges related along with his most cancers, together with results from a stroke, deafness in a single ear that required him to go to a college for deaf college students, and for 3-and-a-half years, a tracheostomy tube that required his mom to journey with a nurse any time she left the home along with her son.
“Medicaid is a important perform for us having the ability to present the care that he wants between the pharmacies and the personal responsibility nursing after which, in fact, the precise care itself that he receives for the acute state of affairs,” mentioned his mom, Erica Olenski Johansen. “I imply, there’s loads concerned, clearly, when you will have a child with medical complexity.
The re-enrollment course of had snagged when Johansen missed the paperwork for renewal over final summer season as a result of she wasn’t in search of it. However her son ought to have maintained his protection as a result of it wasn’t income-based, she mentioned.
In November she acquired discover that he’d be dropped. Her new revenue ranges prevented her from re-enrolling, despite the fact that her revenue wasn’t a think about August’s eligibility. Then on Dec. 1, he misplaced protection and nursing care.
And it wasn’t till then that an HHSC official was in a position to assist her restart his advantages 10 hours later and resume care the next week.
“They had been very apologetic, which I recognize,” she mentioned.
August had one factor going for him, although: A mom who had labored for years within the well being care trade and who was adept at navigating it.
Tons of of 1000’s of Texans weren’t so good at avoiding the bureaucratic landmines.
Texas 2036’s researchers wrote in February that these persistent “administrative limitations” needs to be addressed by lawmakers after they convene in January 2025 for a brand new session and price range cycle. “Texas policymakers may make vital inroads towards lowering the state’s uninsured inhabitants by growing consciousness of the provision of inexpensive well being protection choices, lowering bureaucratic and administrative complexity in the course of the enrollment course of, and bettering the shopper expertise for Texans in search of out protection,” the report says.
In another states, enrollees are given administrative categorical lanes to assist with the unwinding and reapplication course of — like computerized eligibility if the household already qualifies for meals help, for instance.
These in Texas who recall the scramble to enroll youngsters in CHIP in the course of the election season of 2000 say it’s tough now to observe different states make it simpler for certified folks to remain lined — whereas the processes they put in place many years in the past to get so many low-income youngsters lined have fallen by the wayside.
“The surroundings has utterly flipped,” Fritz mentioned. “It’s prefer it’s now not a excessive precedence to get youngsters enrolled and maintain them enrolled. It’s precisely the other. It’s form of like, ‘You’re by yourself, folks.’ That is the place we’re. Is that this the place we wish to be?”
This text initially appeared within the Texas Tribune.
The Texas Tribune is a member-supported, nonpartisan newsroom informing and interesting Texans on state politics and coverage. Be taught extra at texastribune.org.
Subscribe to SA Present newsletters.
Comply with us: Apple Information | Google Information | NewsBreak | Reddit | Instagram | Fb | Twitter| Or join our RSS Feed





